Neurophysiology, neuroradiology, neuropathology Question Bank
Quiz Summary
0 of 24 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 24 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 24
1. Question
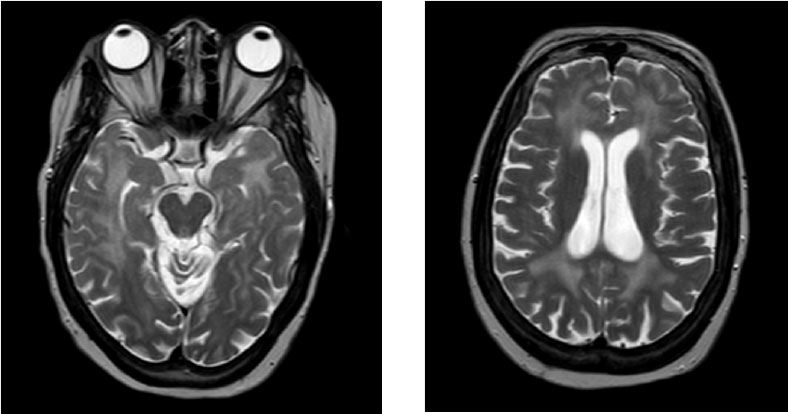
An 18-year-old female had her first seizure 6 months ago. She undergoes an MRI head as part of her work up for epilepsy. She has no other neurological symptoms or signs and no significant past medical history.
What is the most likely diagnosis based on the presentation and MRI findings?
 CorrectIncorrect
CorrectIncorrect -
Question 2 of 24
2. Question
A 58-year-old male presented with a 4-day history of progressive and fluctuant bilateral lower limb weakness and paraesthesia with urinary retention. Past medical history was notable only for hypertension. His condition appeared to deteriorate following intravenous corticosteroids.
He underwent an MRI spine – cervical and upper thoracic sagittal imaging is shown below.

Which of the following investigations is most likely to confirm the diagnosis?
CorrectIncorrect -
Question 3 of 24
3. Question
A 20-year-old female presented with new-onset status refractory status epilepticus. On the day of admission, she complained of headache and vomited.
She had a history of low mood and 2 days previously had been treated for paracetamol overdose and discharged.
Examination off sedation revealed complex ophthalmoplegia and bilateral ptosis.
CSF examination showed WCC 1/mm3 (negative gram stain and negative standard viral PCR), protein 0.4g/L, glucose 4.1 mmol/mol.
Axial T2 (A) and axial diffusion-weighted (B) MRI are below.

What is the most likely diagnosis?
CorrectIncorrect -
Question 4 of 24
4. Question
A 35-year-old woman is referred to the Emergency Neurology clinic by her GP. She reports a 3-day history of back pain, ascending numbness and lower limb weakness.
She has a history of Ro antibody-positive Sjogren’s disease and a provoked lower limb DVT following a Caesarean section 3 years prior. She is on vitamin B12 supplements after an incidental finding of macrocytic anaemia but no other medications.
On examination, cranial nerves are intact with normal visual acuity and healthy optic discs. Upper limb examination is remarkable for brisk reflexes and mild symmetrical weakness of finger flexion and abduction. Lower limb examination reveals a moderate spastic paraparesis with hyperreflexia and extensor plantar responses. She has a sensory level to pin-prick at the level of T2.
You arrange an urgent MRI spinal cord, shown below.

What is the most likely cause of her presentation?
CorrectIncorrect -
Question 5 of 24
5. Question
A 42-year-old man presents to his local emergency department with 3 severe headaches in the past week. Today, the headache was accompanied by twitching of the right arm and leg and visual disturbance affecting his right hemifield. Twitching resolves with intravenous lorazepam and a mild left hemiparesis and visual deficits persist.
He has a history of oligodendroglioma treated with surgery and chemoradiotherapy 8 years previously. He had seizures at the time of diagnosis but none for 8 years. He takes levetiracetam 750mg BD but admits to poor compliance. CT angiography is normal.
MRI brain showed an area of cortical swelling and high T2 signal in the left occipital lobe extending to the adjacent parietal lobe, which enhanced with contrast (see below).
4 weeks later he continues to experience intermittent right sided twitching but headaches, visual disturbance and weakness have resolved. A repeat MRI demonstrates partial resolution of the changes (not shown).

Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 6 of 24
6. Question
In relation to radiation-induced tumours of the nervous system, which of the following statements is correct?
CorrectIncorrect -
Question 7 of 24
7. Question
A 29-year-old female presents with a 24-hour history of fluctuating confusion, headache, visual hallucinations and seizures. Paramedics described some writhing movements. In the Emergency Department she is treated for status epilepticus and intubated. She is febrile and tachycardic.
You are called to the intensive care unit the next day due ongoing seizure activity despite repeated doses of lorazepam, loading with 4g of levetiracetam and sedation with propofol. You note facial grimacing and intermittent limb jerking on the left.
Toxicology screen is negative. CSF shows moderate lymphocytosis with a negative gram stain and a negative viral PCR. MRI (axial T2 and coronal flair) is shown below.

What is the most likely diagnosis?
CorrectIncorrect -
Question 8 of 24
8. Question
A 62-year-old gentleman present to the Emergency Department with sudden left-hand weakness.
He has a normal CT brain and proceeds to an MRI-brain (see figure, left = DWI; right = ADC map).

What is the diagnosis?
CorrectIncorrect -
Question 9 of 24
9. Question
A 69-year-old female under investigation for cognitive decline by her GP for the last 2 months presents with dysphasia progressing over days to weeks.
She has difficulty following commands and is unable to provide any verbal output. She is generally quite limited in her movements globally. There are no lateralising neurological findings and she is afebrile.
An MRI is performed, with 2 axial DWI images shown below.

What is the most likely diagnosis?
CorrectIncorrect -
Question 10 of 24
10. Question
A 50-year-old female with a 15-year history of HIV is admitted to the infectious disease ward with a history of progressively erratic behaviour and poor organisation for several months. Family have been concerned about her ability to cope at home and also that her medication compliance is poor.
She has no other medical history. She is a lifelong non-smoker and drinks alcohol only rarely.
On examination, she exhibits psychomotor slowing and is apathetic. There are no focal neurological signs.
She declined lumbar puncture. Her HIV viral load is 750 IU/ml.
MRI at presentation is shown below and showed no change in appearance when repeated 4 weeks later. There was no restricted diffusion or abnormal contrast enhancement on other sequences.
What is the most likely diagnosis?
CorrectIncorrect -
Question 11 of 24
11. Question
Which of the following features is NOT characteristic of CT scans in normal pressure hydrocephalus?
CorrectIncorrect -
Question 12 of 24
12. Question
A 42-year-old gentleman presents to The Emergency Department with new-onset focal seizures with secondary generalisation. His past medical history is unremarkable. He reports previous intravenous drug use but he has been clean for ‘many years’. His travel history includes a recent trip to China and Cambodia.
On your arrival he seems to have made a good recovery from his seizures and is conversational.
An MRI-brain is performed and shown below.

What is the diagnosis?
CorrectIncorrect -
Question 13 of 24
13. Question
A 19-year-old man is admitted to hospital following a head injury 2 hours ago while playing rugby. A blow to the head was witnessed with a subsequent loss of consciousness for around 5 minutes. He now is tired with a mild headache.
Examination reveals a Glasgow coma score of 15 with no focal neurological deficit. On further questioning with witness corroboration, he exhibits 60 minutes of retrograde amnesia.
What is the most appropriate management?
CorrectIncorrect -
Question 14 of 24
14. Question
A 62-year-old man with Parkinson’s disease undergoes an MRI brain as part of work-up for deep brain stimulation. The scan identifies an asymptomatic incidental meningioma. On review of previous imaging this is noted on a CT brain 2 years previously and has not changed in size or appearance.
Which of the following is correct with respect to NICE guidance on radiological surveillance of this meningioma?
CorrectIncorrect -
Question 15 of 24
15. Question
A 3-year-old boy is seen in the Neuropaediatrics Department following witnessed seizures. His parent’s report violent limb jerks lasting seconds, often in bright light, with preserved awareness but also describe events characterised by loss of consciousness with whole body shaking and head turning.
He was born without complication, albeit slightly small for gestational age. He has been otherwise well and reached developmental milestones at the appropriate ages.
On examination, he is short for his age and there is evidence of cerebellar ataxia.
Blood lactate levels and CK are raised and CSF examination is acellular but with a slight raised protein concentration at 0.5g/L and lactate 4mmol/L. An MRI brain reveals cerebellar atrophy and grey matter T2-weighted hyperintensities. EEG reveals a slow background with some generalised epileptiform discharges on photic stimulation.
A muscle biopsy is performed and shown below.

What is the most likely diagnosis?
CorrectIncorrect -
Question 16 of 24
16. Question
A 74-year-old gentleman passed away with pneumonia following an undifferentiated neurodegenerative process. A section from the post-mortem histopathology is shown below.

What is the most likely underlying disease associated with this pathology?
CorrectIncorrect -
Question 17 of 24
17. Question
Which of the following histopathological features are seen in frontotemporal dementia?
CorrectIncorrect -
Question 18 of 24
18. Question
A 62-year-old gentleman presents with progressive painful proximal weakness. A muscle biopsy is performed and shown below.

What is the diagnosis?
CorrectIncorrect -
Question 19 of 24
19. Question
A 72-year-old female is brought to the Emergency Department after being found on the floor with bruising around her face. She was found slumped against her radiator. She lives alone and her house was in disarray.
She has a past medical history of diet-controlled type 2 diabetes and hypertension. There is no history of drug or alcohol use and she is well nourished.
On examination she is confused with a plethoric appearance. Neurologically, she has bilateral extensor plantar responses and some left-sided appendicular ataxia.
An MRI-brain reveals diffusion restriction within the splenium of the corpus callosum.
Which of the following investigation is likely to most help with the diagnosis?
CorrectIncorrect -
Question 20 of 24
20. Question
A 12-month-old boy is brought to the outpatient Paediatric Neurology Department by his parents due to delayed acquisition of motor milestones. His parents report difficulty with head control and he is not crawling.
Examination reveals depressed reflexes, hypotonia and bilateral ptosis.
A muscle biopsy is shown in the figure below.

A mutation in what gene is most likely to be found in this patient?
CorrectIncorrect -
Question 21 of 24
21. Question
A 50-year-old gentleman is admitted with generalised seizures. According to his wife, he had been complaining of a headache for the past fortnight for which he was taking regular paracetamol. He has no significant medical history.
On arrival in the Emergency Department he had a CT-brain, which revealed a left frontal lesion further characterised with an MRI-brain (shown below).

He was subsequently referred to neurosurgery who discussed the case at the regional multidisciplinary team meeting. They decided to proceed with a biopsy of the lesion for histopathological characterisation (shown below).

The tissue is sent for further molecular analysis which reveals an IDH mutation and codeletion of chromosome arms 1p and 19q (also known as 1p/19q codeletion).
Treatment with radiation and chemotherapy is recommended.
What is the cause of this lesion?
CorrectIncorrect -
Question 22 of 24
22. Question
A 64-year-old gentleman is seen in the Emergency Department due to progressive unremitting headache and papilloedema noted by his local optometrist, who advised admission.
He has no past medical history and is a non-smoker.
Neurological examination reveals some mild left-sided weakness and direct fundoscopy confirms the presence of optic disc swelling without haemorrhages.
An MRI-brain is shown below.

He undergoes a brain biopsy and the histology is reviewed by the neuropathologist, who confirms this is a WHO grade IV primary glioblastoma.
Which of the following altered tumour genomic/molecular profiles would support this diagnosis?
CorrectIncorrect -
Question 23 of 24
23. Question
A 12-year-old girl attends your Neurology clinic with progressive unsteadiness, which presented at 5-years-old with clumsiness and falls. She has a history of bilateral toe clawing requiring bilateral cavovarus corrective surgery. There is no history of sensory symptoms, visual alteration or sphincter disturbance.
She is adopted and has no awareness of the health of her biological family history.
Examination reveals broken pursuit but with full range of eye movements and no nystagmus. She exhibits marked upper limb dysmetria and intention tremor and lower limb heel-shin ataxia, hammer toes, vibration loss to the ankles but with other sensory modalities intact. Her tone is spastic in her lower limbs but normal in the arms. Motor testing reveals mild global 4/5 weakness in her lower limbs only. Deep tendon reflexes are generally diminished or absent bilaterally and plantar responses are extensor.
Blood tests including vitamin B12, folate, thyroid function, vitamin E, phytanic acid, paraneoplastic antibodies, calcium channel antibodies, GAD antibodies, coeliac screen, lactate, copper, caeruloplasmin, cholestanol, and coenzyme Q10 are all negative or normal. An MRI-brain is shown below.

Nerve conduction studies (NCS) are arranged demonstrating prolonged distal latencies with decreased motor velocities in all limbs. Sensory NCS were unrecordable. In view of this presentation, fundal photographs and optic coherence tomography are performed which confirm retinal nerve fibre layer thickening.
What is the likely diagnosis?
CorrectIncorrect -
Question 24 of 24
24. Question
A patient is being worked-up for an undifferentiated progressive sensory and motor peripheral neuropathy and undergoes a nerve biopsy (shown below).

Which of the following are associated with this appearance?
CorrectIncorrect

In the question of identification of biopsy result in ‘A 62-year-old gentleman presents with progressive painful proximal weakness.’ What are the histological features there to speak against necrotising myositis?
Thanks very much for your query. The histopathological hallmark is the presence of randomly distributed necrotic muscle fibres along with fibres in various stages of regeneration, but in the absence of or sparse mononuclear cell infiltrates.