Management (neurosurgery, intensive care neurorehabilitation, clinical pharmacology) Question Bank
Quiz Summary
0 of 30 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 30 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 30
1. Question
Which of the following medications predominantly blocks calcium channels as its mechanism of action?
CorrectIncorrect -
Question 2 of 30
2. Question
An 82-year-old patient with advanced stage Parkinson’s disease (PD) is referred for an inpatient neurology review. He has become confused following a recent change in his Parkinson’s medications. There are no other medications contributing to his symptoms and no acute medical concerns otherwise. Routine blood tests and a urine dip are normal with no evidence of infection.
You are asked to rationalise his medication to help mitigate these side effects. Which of the following is the first medication that you would consider stopping?
CorrectIncorrect -
Question 3 of 30
3. Question
Which of the following medications is a weak inhibitor of carbonic anhydrase?
CorrectIncorrect -
Question 4 of 30
4. Question
A 62-year-old male has been admitted with a brief history of visual disturbance and headache shortly followed by confusion and seizures.
His examination reveals a GCS of 9 (M4V3E2) but he is maintaining his airway. He has a temperature of 37.6C, pulse 80bpm (regular), blood pressure 192/110mmHg, respiratory rate 18 and oxygen saturations of 88% on room air. A retinal examination reveals some copper wiring, cotton wool spots and A-V nipping without haemorrhages or papilloedema.
An MRI scan is shown below.

Which medication can cause this condition?
CorrectIncorrect -
Question 5 of 30
5. Question
Which of the following anti-seizure medications is least likely to worsen childhood absence epilepsy?
CorrectIncorrect -
Question 6 of 30
6. Question
Which of the following anti-seizure medications has the most significant impact on blood hormonal levels and may reduce the effectiveness of the combined oral contraceptive pill?
CorrectIncorrect -
Question 7 of 30
7. Question
A patient is admitted to the neurology ward with proximal lower limb weakness, ataxia, autonomic features. At rest he is areflexic but reflexes appear after isometric muscle contraction.
He is diagnosed with Lambert-Eaton myasthenic syndrome (LEMS), after which he receives acute immunotherapy and is started on 3,4-diaminopyridine.
What is the mechanism of action of 3,4-diaminopyridine?
CorrectIncorrect -
Question 8 of 30
8. Question
A 52-year-old male is admitted under the neurosurgeons with suspected cauda equina syndrome.
An urgent spinal MRI reveals a discontinuous T2 cord hyperintensity in the lower thoracic cord extending to the conus with smooth, linear nerve root enhancement but no surgical cauda equina syndrome.
He has no significant past medical history beyond recent genital ulcers. He has no mouth ulcers and a pathergy test is negative. There are no skin changes.
A CSF is examined which demonstrates a lymphocytic pleocytosis with no oligoclonal bands.
What is the most likely diagnosis?
CorrectIncorrect -
Question 9 of 30
9. Question
A 60-year-old male with idiopathic Parkinson’s disease diagnosed 5 years ago is being considered for deep brain stimulation.
Which of the following is a correct indication?
CorrectIncorrect -
Question 10 of 30
10. Question
A 62-year-old gentleman is being considered for a decompressive hemicraniectomy 52 hours following a proximal left M1 occlusion. He has a past medical history of diabetes, hypertension and is a lifelong smoker.
His National Institutes of Health Stroke Scale (NIHSS) score is 19, consciousness is decreased and he has evidence of an infarction involving 75% of the middle cerebral artery territory.
As per NICE guidance, which of the above are contraindications to decompressive hemicraniectomy?
CorrectIncorrect -
Question 11 of 30
11. Question
Which of the following is required as part of the diagnosis of brainstem death within the UK for adults?
CorrectIncorrect -
Question 12 of 30
12. Question
A 43-year-old male is brought to hospital with an acute onset headache and an episode of vomiting.
On examination, he is alert and able to obey commands but is not oriented in place or time. Pupils are equal and reactive to light. He has a left upper motor neuron facial droop. There are no bulbar deficits. Right-sided limb power is 5/5 on the MRC scale but is 3/5 throughout on the left with a flaccid hemiparesis.
A CT scan confirms a subarachnoid haemorrhage.
According to the World Federation of Neurological Surgeons Subarachnoid Haemorrhage grading scale, what is the grade of the severity of the bleed?
CorrectIncorrect -
Question 13 of 30
13. Question
A 23-year-old woman is brought to the Emergency Department with a debilitating headache. She describes a sudden onset occipital pain 45 minutes ago. On direct questioning, she is sensitive to light and nauseated but has not vomited. She denies head trauma or recreational drug use.
She has a history of depression and occasional sinusitis and attended hospital 6 weeks ago for a similar headache. She takes 100mg sertraline OD and oral decongestant PRN.
On examination, GCS is 15. She is clearly uncomfortable but is not meningitic. Cranial nerve, upper and lower limb examinations are normal.
An urgent CT scan is requested and is shown below.

Which of the following statements is true?
CorrectIncorrect -
Question 14 of 30
14. Question
A 42-year-old man with secondary progressive MS is brought to Accident and Emergency by his carer. He was diagnosed with relapsing remitting MS 15 years previously and was initially treated with beta interferon, but high disease activity prompted a switch to natalizumab. This was discontinued 3 years ago due to high anti-JC virus antibody titres. He was then switched to ocrelizumab. His last infusion was 4 months ago. His last relapse was 5 years ago with a partial transverse myelitis.
His baseline EDSS is 6.5 and a carer visits three times a day to help with self-care and meal preparation. He has an indwelling catheter and a baclofen pump for severe lower limb spasticity.
Medications, other than those mentioned above, include gabapentin 600mg TDS for pain, amitriptyline 100mg ON for pain and low mood, and prophylactic nitrofurantoin for recurrent urinary tract infections.
His carer describes a 24-hour history of rapidly progressive confusion and fever. He has omitted his usual medications today.
On examination, he is disoriented with evidence of paranoid ideation. He is flushed and diaphoretic with a low-level tachycardia (120 bpm), hypertension (180/100 mmHg) and fever (39.2°C). His chest is clear and his abdomen is soft. There is no abdominal tenderness. Neurological examination reveals a GCS of 14 (E4V4M6) with tremor, severe spasticity in all limbs and hyperreflexia. He has a sensory level at T10.
Blood tests reveal a normal haemoglobin level with lymphopaenia and acute kidney injury with elevated creatine kinase.
What is the most important aspect of his immediate management?
CorrectIncorrect -
Question 15 of 30
15. Question
A 64-year-old woman is brought to Accident and Emergency by ambulance. She was seen well 8 hours ago by her son and was found 30 minutes ago by her friend with a right hemiplegia and expressive dysphasia.
On examination, she is normotensive and alert. NIHSS is shown below:
Item Score 1a (LOC responsiveness) 0 1b (LOC questions) 1 1c (LOC commands) 0 2 (Eye movement) 2 3 (Visual fields) 2 4 (Facial palsy) 1 5 (Motor arm) 2 right, 0 left 6 (Motor leg) 2 right, 0 left 7 (Limb ataxia) 0 8 (Sensory) 1 right, 0 left 9 (Language) 1 10 (Speech) 1 11 (Inattention) 0 Medical history includes well-controlled type 2 diabetes mellitus and hypertension.
A CT confirms a large left middle cerebral artery (MCA) infarct affecting approximately half of the artery’s territory. There is also a small infarct affecting approximately 20% of the territory of the ipsilateral anterior cerebral artery. CTA does not reveal any causative thrombus.
There are no contraindications, so she receives thrombolysis and is taken to the Stroke ward.
18 hours later she deteriorates. 1b on the NIHSS increases to 2 (unable to answer any question), 1c increases to 1 (performs only 1 of 2 tasks deteriorated). Facial palsy is more marked (2) and right arm is weaker (3). Language deteriorates to the point of incomprehensibility (2). She has an urgent CT scan, confirming worsening left hemisphere oedema.
Which of the following statements is true?
CorrectIncorrect -
Question 16 of 30
16. Question
A 42-year-old man attends the Accident and Emergency Department in acute urinary retention. You are asked to review the patient, as he reported a 2-day history of lower back pain and bilateral leg weakness.
Other than hypertension, medical history is unremarkable. He takes only ramipril. His father was diagnosed with primary progressive multiple sclerosis aged 50.
On examination, he is now catheterised. Lower limb tone is normal without ankle clonus and there is bilateral symmetrical leg weakness, MRC grade 4 at the hip and knee and 3 at the ankle. Reflexes are absent and plantar responses are mute. There is a sensory level at the pelvis with saddle anaesthesia.
An MRI of the lumbar spine with gadolinium shows no compression but smooth enhancement of the cauda equina nerve roots. A CSF sample sent by the Acute Medical Team reveals a mild mixed pleocytosis (80% lymphocytes, 20% neutrophils) with a moderately increased protein concentration (0.92 g/dL) and a normal CSF:serum glucose ratio.
What of the following tests is most likely to be diagnostic?
CorrectIncorrect -
Question 17 of 30
17. Question
You are reviewing a patient on ICU with proven meningococcal meningitis.
An MRI scan performed 2 days prior revealed marked cerebral oedema.
In light of upper motor neuron signs and bilateral papilloedema, an external ventricular drain was placed to monitor intracranial pressure. Intracranial pressure is 35mmHg and mean arterial pressure is with vasopressor support is 85mmHg.
Which of the following statements is true?
CorrectIncorrect -
Question 18 of 30
18. Question
You are asked to provide a prognosis for a 65-year-old woman on ICU. She suffered a witnessed cardiac arrest in the community 4 days prior. A bystander commenced CPR almost immediately and resuscitation was continued by the paramedics on arrival, with an estimated 16 minutes between loss of output and return of spontaneous circulation.
Her initial rhythm, recorded by the paramedics at 5 minutes after collapse, was ventricular fibrillation and 3 shocks were administered.
When you examine her on ICU, she is intubated and ventilated. Her pupils are not responsive to light and she does not blink in response to corneal stimulation. Tone is increased in arms and legs and plantar responses are extensor. She has no response to supraorbital pressure.
You request electrophysiological studies. An EEG shows generalised suppression. Visual evoked potentials show no cortical response to chequerboard patterns and somatosensory evoked potentials show no N20 cortical response to median nerve stimulation. An MRI obtained the same day shows generalised oedema with blurring of the grey-white matter borders.
Which of the following combinations of features most accurately predicts poor outcome (death or persistent unconsciousness) in this patient?
CorrectIncorrect -
Question 19 of 30
19. Question
A 32-year-old male with post-traumatic epilepsy dating from an accident 3 years ago is brought to hospital with ongoing generalised tonic seizure activity.
By the time of arrival, 35 minutes after seizure onset, he has received a total of 12mg IV lorazepam and seizures persist. He is given 3g IV valproate. Clinical seizure activity ceases but he fails to wake and there is concern he is in non-convulsive status epilepticus. He is therefore intubated, transferred to ITU and started on a propofol infusion (0.1mg/kg/min) with his usual levetiracetam 1.5g BD continued.
Twenty-four hours later, propofol is stopped and seizures re-emerge. Propofol is restarted and valproate 1g BD IV is added.
After a further 24 hours, cardiac monitors show a decline in heart rate to 42 bpm and an ECG confirms bradycardia with a prolonged PR interval. Blood tests are shown below:
Serum parameter Concentration Normal values Sodium (mmol/L) 145 135 – 135 Potassium (mmol/L) 6.2 3.5 – 5.5 Urea (mmol/L) 8.8 2.5 – 7.5 Creatinine (micromol/L) 534 60 – 110 ALT (IU/L) 45 10 – 60 ALP (IU/L) 124 30 – 130 pH 7.31 7.35 – 7.45 Creatine kinase (IU/L) 860 40-320 An infusion of insulin and dextrose is started and the rate of fluids is increased.
What is the correct next step?
CorrectIncorrect -
Question 20 of 30
20. Question
Which of the following features of meningioma is associated with a poor prognosis?
CorrectIncorrect -
Question 21 of 30
21. Question
Which of the following drugs may cause a myasthenic crisis in individuals with myasthenia gravis?
CorrectIncorrect -
Question 22 of 30
22. Question
An 82-year-old gentleman with Parkinson’s disease describes postural dizziness following commencement of a new medication.
Which of the following is most likely contributing to his orthostatic hypotension?
CorrectIncorrect -
Question 23 of 30
23. Question
Which of the following statements regarding treatment of status epilepticus in the landmark ESETT trial is true?
CorrectIncorrect -
Question 24 of 30
24. Question
According to the World Health Organisation, which one of the following is included in the clinical criteria of mild traumatic brain injury?
CorrectIncorrect -
Question 25 of 30
25. Question
An elderly gentleman presents to the hospital following an unwitnessed fall with severe headache, vomiting, and altered level of consciousness.
On examination, the patient has a dilated and unresponsive right pupil, and left-sided hemiparesis.
What herniation syndrome is this?
CorrectIncorrect -
Question 26 of 30
26. Question
A patient’s brain biopsy is being discussed at the weekly neurosurgical multi-disciplinary team meeting. The neuropathology is shown below.
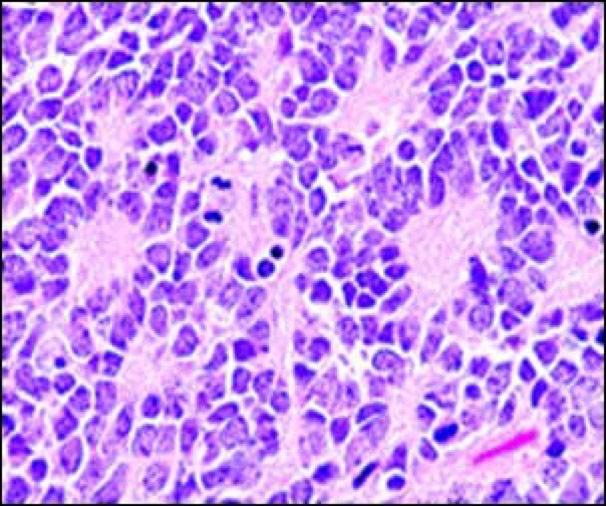
Which of the following is the most likely brain tumour in question?
CorrectIncorrect -
Question 27 of 30
27. Question
A 32-year-old female presents to the Emergency Department with sudden-onset severe headache and visual disturbances.
On examination, her heart rate is 72 beats/minute, blood pressure 82/54mmHg, temperature 37.2℃, oxygen saturations 98% on room air and respiratory rate is 12/minute. Neurological examination reveals constriction of both peripheral fields. The remainder of the neurological examination is normal.
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 28 of 30
28. Question
Which of the following is a fully human antibody to the CD20 antigen that is used in the treatment of MS?
CorrectIncorrect -
Question 29 of 30
29. Question
Regarding the pharmacokinetics of levodopa, which of the following statements is correct?
CorrectIncorrect -
Question 30 of 30
30. Question
A 30-year-old lady attends general neurology outpatient clinic with headaches. The diagnosis is consistent with tension type headache. However, she explains that her brother died recently of an aneurysmal subarachnoid haemorrhage (SAH) aged 40 and her mother died of a brain haemorrhage in her late 60s.
She has heard there can be a familial predisposition to aneurysms and asks to be screened.
Which of the following investigations is most appropriate?
CorrectIncorrect
