Disorders of Peripheral Nervous System and Muscle Question Bank
Quiz Summary
0 of 26 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 26 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 26
1. Question
A 25-year-old male presents with a progressive difficulty walking and gradually worsening paraesthesia affecting his feet. There is a family history of similar foot symptoms.
On inspection, pes cavus is present and there is evidence of distal ankle weakness and loss of sensation to pinprick to the mid-shins bilaterally and vibration to the tibial tuberosity. Lower limb reflexes are absent.
Nerve conduction studies reveal conduction velocities of 32m/s in the tibial and 36m/s in the common peroneal nerves (normal values ≥ 38 m/s in both) with distal motor latencies of 7s between abductor hallucis and ankle (normal ≤ 6.5ms) and 7.2s between extensor digitorum brevis and the ankle (normal ≤ 6.5ms).
What is the most likely genetic mutation causing this presentation?
CorrectIncorrect -
Question 2 of 26
2. Question
A 22-year-old female student presents with paraesthesia across the right medial forearm into the ring and little finger. She had been drinking heavily the night before. She had previously had an episode where she dragged her left foot for a period of days, which she noticed after spending a week in long lectures.
On presentation to the neurology clinic there is no focal neurological deficit.
An MRI-brain and cervical spine is normal. A tomaculous neuropathy is suspected.
What is the most likely cause?
CorrectIncorrect -
Question 3 of 26
3. Question
A 67-year-old male is referred with difficulty standing from a sitting position. He also reports dizziness on standing, fatigue and dry mouth. He denies any sensory symptoms or sphincter disturbance. He is a current smoker and past medical history includes type 2 diabetes, hypertension and hypercholesterolaemia. Medications include atorvastatin, amlodipine, metformin, aspirin and insulin.
Examination revealed a supine blood pressure of 140/95mmHg (standing 110/75mmHg), heart rate 85 bpm, respiratory rate 14/min and temperature of 37.1°C. Cranial nerves were normal. Lower limb examination identified hip flexion power 4/5, hip extension 4+/5, knee extension 4+/5, knee flexion 5/5, dorsiflexion 5/5, plantar flexion 5/5 and hallux extension 5/5 bilaterally. Upper limb power was 5/5. Reflexes were diminished globally. Sensory and cerebellar examination was normal.
Investigations revealed a CK of 420U/L (normal range: 10-80U/L), LDH 160U/L (range: 140-280U/L), negative anti-nuclear, anti-acetylcholine receptor, anti-voltage gated calcium and paraneoplastic antibodies. An EMG shows facilitation at 50Hz stimulation, but not at 3Hz.
What is the most likely diagnosis?
CorrectIncorrect -
Question 4 of 26
4. Question
A 6-year-old boy with a diagnosis of slow channel congenital myasthenic syndrome treated with pyridostigmine is reviewed in clinic. His mother reports that his head drops between doses recently.
Examination in clinic reveals weakness of neck flexion, finger and wrist extension.
What is the next step in management?
CorrectIncorrect -
Question 5 of 26
5. Question
A 35-year-old female is reviewed in clinic with a progressive acroparaesthesia in her feet, as well as altered bowel habits. She is otherwise fit and well and takes no regular medications. Her father required a liver transplant and her paternal grandfather died unexpectedly at a young age.
On examination there is spinothalamic sensory lost to the mid-shins bilaterally. Her ankle jerks are absent but the remainder of the neurological examination was satisfactory. Her supine blood pressure was 124/78 (standing 92/60), heart rate 89 bpm, respiratory rate 14/minute and temperature 36.9°C.
What is the most likely diagnosis?
CorrectIncorrect -
Question 6 of 26
6. Question
An EMG investigating the possibility of carpal tunnel syndrome reveals the following results.
Distal latency (t1)= 4ms
Proximal latency (t2) = 9ms
Distance between proximal to distal sites = 20cm
What is the conduction velocity?
CorrectIncorrect -
Question 7 of 26
7. Question
A 65-year-old gentleman is seen in the Emergency Department with a progressive 2-week history of double vision and dysphagia. He has a past medical history of type 2 diabetes mellitus and hypertension. He has recently been started on clarithromycin for a chest infection.
His observations reveal a temperature of 37.6 degrees Celsius, heart rate of 105bpm, blood pressure 100/65mmHg, respiratory rate of 22/min and saturations 94% on room air. His examination reveals some proximal weakness with fatigability including fatigable ptosis on sustained upgaze. His neck flexion is 4/5 on the Modified Research Council (MRC) scale.
He is then referred to Neurology and has nerve conduction studies that show decrement and jitter consistent with myasthenia gravis. He starts treatment with pyridostigmine 30mg QDS.
Which of the following do not aggravate or induce myasthenia gravis?
CorrectIncorrect -
Question 8 of 26
8. Question
A 60-year-old gentleman is admitted with progressive proximal muscle weakness, dry mouth, erectile dysfunction and dizziness. On direct questioning, he reports some unintentional weight loss in recent times.
His observations reveal a temperature of 37.1°C, heart rate of 110bpm, blood pressure 90/62mmHg, respiratory rate of 18/min and saturations 98% on room air. His neurological examination reveals weakness of shoulder abduction 4-/5 which improves to 4+/5 after activity. He is also hyporeflexic throughout.
Which of the following tests, if positive, will support the likely diagnosis?
CorrectIncorrect -
Question 9 of 26
9. Question
A 60-year-old female is admitted to the Emergency Department with a sudden onset weakness of the right-hand. She has a past medical history of rheumatoid arthritis.
Her observations reveal a temperature of 37°C, heart rate of 85bpm, blood pressure 137/92mmHg, respiratory rate of 18/min and saturations 98% on room air. On examination, you notice her wrist extensors on the right are weak with 2/5 on the MRC power scale, reducing further on attempted fist closure. Her elbow extension power is 5/5, her reflexes are normal and sensation is reduced around the first dorsal interossei.
Where is the lesion likely to be within the neuroaxis?
CorrectIncorrect -
Question 10 of 26
10. Question
A 24-year-old female presents with weakness and falls. She was quite clumsy as a child but her motor development was satisfactory. She was born by normal vaginal delivery with no complications. There is a similar presentation in her family; including her children (see figure below). Of note, the male at the top of the family tree is NOT a disease carrier.
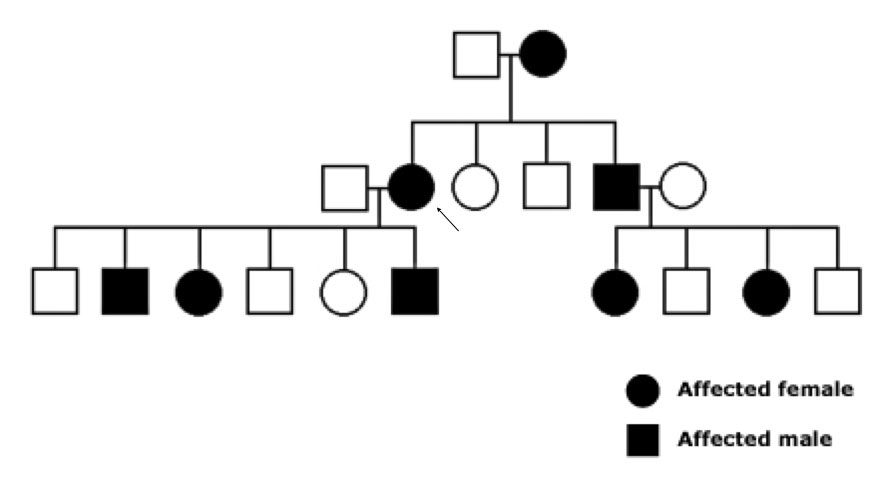
On examination, you notice a foot drop with distal leg wasting and pes cavus. According to the MRC grading scale, ankle dorsiflexion power is 2/5, plantar flexion 4-/5, inversion 4/5, and eversion 3/5 bilaterally. Proximal motor exam was normal. Reflexes were absent throughout and sensation was reduced to the mid-shin to pinprick and light touch. Vibration was reduced to the tibial tuberosity and proprioception to the ankle. Upper limbs and cranial nerves were normal other than sensorineural deafness bilaterally requiring hearing aids.
Nerve conduction studies reveal intermediate conduction velocities, mildly prolonged F waves, and evidence of distal axonal loss. A cerebrospinal fluid examination is arranged which shows WCC=1/mm3, RCC=1/mm3, protein 0.8g/L, glucose 4 mmol/mol (plasma glucose 6).
What is the likely underlying condition?
CorrectIncorrect -
Question 11 of 26
11. Question
A 60-year-old gentleman diagnosed with painful chronic inflammatory demyelinating polyneuropathy (CIDP) has failed two first-line treatments. He has proximal and distal weakness with a severe sensory ataxia.
His blood tests reveal an HbA1C of 41mmol/mol, TSH 0.5 (range: 0.27-4.2mU/L), no paraprotein on serum/urine immunofixation, 2g urinary protein/ 24 hours, positive p-ANCA but negative PR3 and MPO antibodies. He undergoes a renal biopsy, which reveal a membranous glomerulonephritis. Nerve conduction studies reveal reduced motor conduction velocity, prolonged distal motor latencies, decreased CMAP amplitudes and conduction block.
What is the most likely diagnosis in this case?
CorrectIncorrect -
Question 12 of 26
12. Question
A 62-year-old gentleman has been admitted with a progressive 10-week history of distal and proximal limb weakness. His nerve conduction studies and spinal fluid results are consistent with chronic inflammatory demyelinating polyneuropathy (CIDP).
Which of the following treatments has the best evidence of efficacy in CIDP?
CorrectIncorrect -
Question 13 of 26
13. Question
A 23-year-old male was admitted to hospital following a fall and acute weakness. He was noted to have mild limb weakness and you are asked to review him urgently.
He has no past medical history. During his school years he mentioned he found it difficult to play with his friends at lunch as he would feel weak for hours to days after exertion. This recurred in a similar but not wholly stereotypical fashion and could also be triggered by starchy meals. There is a family history of a similar phenotype in his father and paternal grandmother.
His examination showed subtle power reduction (MRC grade 4/5) in all four limbs with absent reflexes and no evidence of myotonia. Hoover’s test was negative. Sensory exam was normal and during the latter part of the examination, his power returned to normal.
There were no dysmorphic features and his ECG did not reveal any conduction abnormalities. Blood tests revealed a CK of 800IU/L with a normal potassium, TSH and renal function. White cell enzymes are pending. A standard EMG and nerve conduction studies are normal without evidence of myotonia.
What is the likely diagnosis?
CorrectIncorrect -
Question 14 of 26
14. Question
A 21-year-old male is referred to your clinic due to episodic weakness. He has no past medical history. During his school years he found it difficult to play with his friends at lunch given subsequent weakness. This recurred in a similar but not wholly stereotypical fashion lasting minutes-hours. He also identified cold weather and eating tomatoes and potatoes as triggers.
His examination was normal with no evidence of myotonia. There were no dysmorphic features or muscle hypertrophy and his ECG did not reveal any conduction abnormalities.
Blood tests reveal a normal CK, potassium, TSH and renal function. White cell enzymes are pending. A standard EMG and nerve conduction studies are normal acutely without evidence of myotonia. A long exercise test revealed a 40% reduction in the compound muscle action potential at the abductor digiti minimi after 50 minutes of repeated exercise.
What is the likely diagnosis?
CorrectIncorrect -
Question 15 of 26
15. Question
A 32-year-old male presents to the outpatient department with long-standing but progressive muscle cramps and stiffness. He has no past medical history, takes no regular medications beyond occasional ibuprofen and denies recreational drug use.
On closer questioning, he reports stiffness predominantly in his legs on prolonged rest or sitting (especially after activity) which improves with exercise. It is also affected by extremes in temperature. He is estranged from his immediate family and is, therefore, unaware of any relevant family history.
On examination, there is evidence of gastrocnemius muscle hypertrophy and myotonia which improves with repetition. There is no muscle weakness. The remainder of the neurological exam is normal, as is the cardiovascular exam and there are no abnormal facial phenotypic features. An EMG reveals evidence of myotonic discharges. His ECG is normal.
Which of the following is most likely?
CorrectIncorrect -
Question 16 of 26
16. Question
An 18-year-old barber presents to the Neurology Outpatient Clinic with a three-year history of progressive upper and lower limb weakness. He initially found walking upstairs and uphill difficult, which progressed to difficulty walking on flat and an inability to run. He now has to use his upper limbs to assist when standing from a sitting position and finds it difficult to keep his arms elevated when cutting clients’ hair.
He is otherwise fit and well. He participated in sports up until the age of 15. His father is estranged but is said to have walking difficulties.
On examination there is bilateral wasting of his deltoid and bicep muscles, with scapular winging. There is bilateral proximal upper limb weakness. Examination of the lower limbs demonstrated prominent wasting of the posterior thigh muscles and hip adductors. He was proximally weak in both lower limbs. Neurological and systemic examination were otherwise normal.
His ECG demonstrated normal sinus rhythm. His creatine kinase was >9000U/L.
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 17 of 26
17. Question
A 52-year-old man is seen in the acute medical unit after being admitted with falls and light-headedness. His past medical history includes obstructive sleep apnoea, for which he intermittently uses a CPAP machine. On closer questioning, he reports a fever, weight loss and a flu-like illness several weeks ago. More recently, he has developed early satiety, constipation and light-headedness on getting out of bed.
His examination reveals a heart rate of 92 beats per minute, lying blood pressure 130/90mmHg and standing blood pressure 101/74mmHg, respiratory rate 20/minute and temperature 37.2°C. An ECG reveals normal sinus rhythm. Neurologically, his examination is unremarkable other than bilateral Adie’s pupils. Basic blood tests are unrevealing.
Which test is most likely to reveal the diagnosis?
CorrectIncorrect -
Question 18 of 26
18. Question
A 14-year-old female is seen in outpatient clinic with progressive weakness. She has a history of retinal vasculopathy and kyphoscoliosis. She takes no regular medications but admits to smoking ‘occasional’ marijuana. At school, she has struggled to keep up with her peers in physical education for many years.
On your examination, you notice she has a wide-eyed appearance, asymmetrical smile, sloped shoulders, scapular winging, prominent axial creases, asymmetric bicep atrophy and a protuberant abdomen. There are no visible contractures. Attempted shoulder abduction is slow and results in poly-hill sign. On sitting up, Beevor’s sign is positive. Eyelid closure is weak.
Power examination is detailed below (R;L):
Shoulder abduction 4/5; 4/5
Shoulder adduction 4+/5; 4/5
Elbow flexion 3/5; 4-/5
Elbow extension 3/5; 3/5
Wrist extension 3/5; 3/5
Wrist Flexion: 4/5; 4/5
Finger extension: 3/5; 3/5
Finger flexion: 4/5; 4+/5
First dorsal interossei: 4-/5; 4-/5
Abductor policis brevis: 4-/5; 4-/5
Abductor digiti minimi: 4/5; 4/5
Hip flexion: 3/5; 4+/5
Hip extension: 5/5; 5/5
Hip abduction: 5/5; 5/5
Hip adduction: 5/5; 5/5
Knee flexion: 3/5; 5/5
Knee extension: 3/5; 4+/5
Ankle dorsiflexion: 2/5; 4-/5
Ankle plantar flexion: 5/5; 5/5
Ankle inversion: 4/5; 5/5
Ankle eversion: 4+/5; 5/5
Hallux extension: 2/5; 2/5
Serum creatine kinase is 180U/L (normal 30-145U/L) and EMG reveals small polyphasic motor units with occasional fibrillations and positive sharp waves. Her ECG reveals normal sinus rhythm.
What is the likely diagnosis?
CorrectIncorrect -
Question 19 of 26
19. Question
Regarding chemotherapy-induced peripheral neuropathy, which of the following is incorrect?
CorrectIncorrect -
Question 20 of 26
20. Question
Which of the following is a congenital myopathy that presents in early childhood with muscle weakness and wasting predominantly affecting the distal arms and legs, joint contractures (especially of the elbows and knees), and hypermobility of the hands and feet?
CorrectIncorrect -
Question 21 of 26
21. Question
A 32-year-old man is suffering hand weakness following shoulder, neck and side pain which came on after he exhibited a flu-like illness. The pain has subsided but his weakness remains.
On examination, you note weakness in flexion of the thumb and index finger. Sensation is preserved on all surfaces of the hand.
Which nerve is affected here?
CorrectIncorrect -
Question 22 of 26
22. Question
A 68-year-old man reports a 3-year history of difficulty rising out of low chairs and struggling to climb stairs without a handrail. In the last year he has had 4 completed falls. He has difficulty opening jars and mild difficulty swallowing solids.
Cranial nerve examination is normal but there is mild weakness of neck flexion. There is wasting and mild-moderate asymmetric weakness in the distal forearms, proximal lower limbs and ankle dorsiflexors. The reflexes are depressed. There are no fasciculations, sensory deficits or cutaneous changes.
Full blood count, renal function, fasting glucose, plasma viscosity, C-reactive protein, serum protein electrophoresis, creatine kinase and thyroid function testing are normal.
Electromyography demonstrates extensive fibrillation potentials and positive sharp waves in the distal muscles of all limbs.
A muscle biopsy is performed and demonstrates the following histochemical features:

a) Congo red staining visualised under florescent light, b) tubulofilaments observed under electron microscopy, c) immunohistochemical staining showing increased sarcolemmal and sarcoplasmic MHC Class I expression, d) sarcoplasmic p62 immunoreactive aggregates, e) TDP-43 immunoreactive aggregates with loss of normal myonuclear TDP-43.
What is the most likely diagnosis?
CorrectIncorrect -
Question 23 of 26
23. Question
A 58-year-old man presents with a 2-day history of double vision, slurred speech and difficulty swallowing. He had been unwell for the last week with a flu-like illness. Past medical history includes Waldenström’s Macroglobulinaemia treated with Rituximab 2 years previously, IgM kappa paraprotein and type 2 diabetes. He reports mild sensory loss in his feet and occasional unsteadiness for the last year for which he has not sought medical attention.
Examination is notable for complex ophthalmoplegia, facial diplegia, dysarthria, mild four limb weakness, global areflexia and distal proprioceptive and vibration loss and gait ataxia.
Routine blood tests are normal aside but there is evidence of Cold agglutinins. Total IgM levels are raised at 6.8g/L. CSF analysis reveals no organisms or cells, protein 0.8 g/L, negative flow cytometry and cytology. Nerve conduction studies demonstrate evidence of demyelination with motor conduction block, prolonged distal motor latencies and reduced conduction velocities.
Anti-ganglioside antibody panel subsequently demonstrated IgM titres of GD1a, GD1b and Gq1b all >1000 (<500).
What is the most likely diagnosis based on the available information?
CorrectIncorrect -
Question 24 of 26
24. Question
A 30-year-old man woke 2 week ago with left hand weakness. There has been no progression and possibly some improvement in the last week. He has no significant past medical history and takes no regular medications.
On examination, there is mild weakness of elbow flexion on the left with moderate weakness of wrist and finger extension and full power in all other arm muscle groups including elbow extension. Reflexes are normal. Sensory examination shows a small area of sensory loss over the anatomical snuffbox on the left. Lower limb examination is normal.
What is the most likely site of the lesion?
CorrectIncorrect -
Question 25 of 26
25. Question
A 10-year-old boy is referred to the Paediatric Neurology clinic for assessment of gradually progressive weakness. He was born at term without complication. However, feeding was poor and motor milestones were delayed (sitting independently at 14 months, walking at 24 months). Speech was also delayed and dysarthric.
From the age of 2 years, he suffered repeated respiratory tract infections. He has required nocturnal ventilation since age 6. He is able to mobilise short distances but requires a wheelchair for use outside. There is no family history of neuromuscular disease.
On examination, he has marked bilateral facial weakness and a high-arched palate. Eye movements are normal. There are contractures involving both hands and ankles and he has mild scoliosis. Assessment reveals weakness of neck flexion and extension and a non-pyramidal pattern of weakness, more marked proximally than distally. Sensation is intact to all modalities.
You suspect a myopathy and request a muscle biopsy. The trichrome-Gomori-stained specimen is shown below:

What is the most likely diagnosis?
CorrectIncorrect -
Question 26 of 26
26. Question
A 42-year-old lawyer is referred to the Neurology clinic with left-sided foot drop.
On examination, lower limb tone is normal. Power according to the MRC scale is tabulated below. Knee and ankle reflexes are intact. Sensation is diminished along the anterolateral calf and dorsal foot, sparing the sole.
Power on MRC scale (/5) is tabulate below:
Muscle action Power right Power left Hip flexion 5 5 Hip extension 5 5 Hip abduction 5 5 Hip adduction 5 5 Knee flexion 5 5 Knee extension 5 5 Dorsiflexion 5 2 Plantarflexion 5 5 Ankle inversion 5 5 Ankle eversion 5 2 Extensor hallucis 5 2 You request nerve conduction studies. These demonstrate acute denervation of the short head of biceps femoris, fibularis (peroneus) longus and extensor hallucis brevis.
What is the site of the lesion?
CorrectIncorrect
