Neurogenetics, neuroendocrinology, neurotoxicology Question Bank
Quiz Summary
0 of 28 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 28 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- Current
- Review / Skip
- Answered
- Correct
- Incorrect
-
Question 1 of 28
1. Question
A 28-year-old female presents to neurology outpatients with progressive painless visual decline. She has no relevant past medical history and reports a normal diet. There is no clear family history. On further questioning, her vision has deteriorated over the past year, beginning in her right eye and later involving her left. She denies headache or pulsatile tinnitus.
On examination, her BMI is 26 and blood pressure 135/86mmHg. Her optic discs are pale, visual acuity 20/200 with reduction in red-green colour vision and contrast sensitivity. The remainder of the neurological examination is normal.
Her Humphrey visual fields are shown below. Her retinal nerve fibre layer reveals temporal sectoral thinning. An MRI brain and venogram is normal. A CSF is pending.

What is the likely cause for her visual decline?
CorrectIncorrect -
Question 2 of 28
2. Question
A 32-year-old female presents to the first fit clinic following a cluster of seizures which abated within 24 hours. She also presents a 2-year history of instability, falls, abnormal movements and progressive cognitive impairment. There is a family history of a similar presentation in her father and paternal grandmother but she is unaware of their diagnosis.
On examination you note some hyperkinetic limb movements consistent with chorea. She has a broad-based gait with appendicular ataxia. An Addenbrooke’s cognitive assessment revealed a score of 50/100, with deficits across all cognitive domains.
Her MRI revealed pontocerebellar atrophy.
A mutation in which of the following genes is the most likely cause?
CorrectIncorrect -
Question 3 of 28
3. Question
You have received the genetics reports for a patient you suspect has Huntington’s disease. What is the minimum number of ‘CAG’ trinucleotide repeats that would definitely confirm your suspicion?
CorrectIncorrect -
Question 4 of 28
4. Question
A 52-year-old gentleman presents to the outpatient clinic with a progressive 3-year history of unsteadiness. He has a past medical history of hypertension and idiopathic peripheral neuropathy. His current medications include amlodipine, ramipril and over-the-counter medication for a chronic cough which started in his twenties. On closer questioning, he describes progressive imbalance, which is worse in the dark, progressive loss of feeling in his feet with paraesthesia and the sense that objects appear to oscillate when turning his head. He also reports dizziness on standing, erectile dysfunction and chronic constipation.
On examination, he had a broad-based gait with evidence of a length-dependent sensory neuropathy with absent ankle jerks but preserved muscle strength. Romberg’s test and head impulse test (bilaterally) were both positive. There was also evidence of intention tremor, dysmetria and dysdiadochokinesia. Eye movements revealed gaze-evoked horizontal and downbeat nystagmus with broken pursuit and dysmetric saccades.
An MRI-brain reveals cerebellar atrophy, predominantly of the vermis. Nerve conduction studies reveal reduced amplitude sensory action potentials with normal motor studies. Blink and masseter reflexes are impaired. An array of aetiological blood tests are negative or normal. You suspect a genetic cause.
Which of the following gene mutations is most likely?
CorrectIncorrect -
Question 5 of 28
5. Question
A 43-year-old French-Canadian female presents to the outpatient clinic with progressive eyelid drooping and dysphagia. She has no past medical history and takes no regular medications. Closer questioning reveals no diplopia and she denies any variation in symptoms. She thinks one of her siblings may have a similar condition but she was adopted and does not know an extensive family history.
Blood tests reveal a mildly raised creatine kinase 300UI/L (normal 100UI/L) with anti-acetylcholine receptor antibodies and anti-MuSK antibodies pending.
On examination, the patient exhibited an imperious look secondary to bilateral ptosis. Her extra-ocular movements revealed a complex ophthalmoplegia without fatigability and her swallowing time extended past 7 seconds when drinking 80mL of ice-cold water. There was no muscle weakness or fatigability.
EMG revealed no decrement and single fibre no jitter.
What is the likely cause of her symptoms?
CorrectIncorrect -
Question 6 of 28
6. Question
A 15-year-old right-handed female is seen in your outpatient clinic with her mother, following recurrent attacks of abnormal speech. She has a past medical history of epilepsy and is maintained on lamotrigine 75mg twice daily. She denies recreational drug use. There is a paternal family history of epilepsy. Her developmental history was notable for a ventouse delivery at term with no additional complications. Age-appropriate milestones were met and she has progressed well through mainstream education. There was no history of meningoencephalitis or febrile convulsions. There were no significant head injuries. On closer questioning, her mother reports hearing banging come from her room at night on a few occasions and when she went to investigate it had stopped, although her daughter seemed very confused on waking and the bed was often wet.
Her epilepsy semiology typically comprises a brief vacant stare followed by an ictal cry and secondary generalisation. Occasionally she had auditory auras prior to the events, when she hears bells ringing in both ears. Similar auditory auras are reported by her father.
The recurrent attacks of abnormal speech involve brief episodes of expressive and receptive language dysfunction with altered awareness. They occur every fortnight.
Her neurological examination in clinic was normal.
A standard EEG is normal with overnight ambulatory EEG showing an interictal spike-wave complex and occasional slow activity over the left temporal region.
Lamotrigine was increased to 100mg twice daily, which abated the events.
What is the most likely underlying cause?
CorrectIncorrect -
Question 7 of 28
7. Question
A 41-year-old South African male attended outpatient clinic with imbalance and cognitive symptoms, depression and irritability. He has a past medical history of diabetes and is maintained on metformin. He has a family history of a similar disorder in his mother and maternal grandfather without a clear diagnosis and passed away when he was young.
On examination, there was a generalised hyperkinetic movement disorder consistent with chorea and a rest tremor with bradykinesia in the upper limbs. Reflexes are brisk and cranial nerves reveal slowing saccades with some ocular dysmetria. There are no cerebellar signs. An Addenbrooke’s III score is 75 with deficits in a subcortical pattern.
An MRI-brain reveals atrophy of the caudate and cortex with brainstem and cerebellar sparing. Blood tests reveal a normal copper, caeruloplasmin and blood film. Genetic testing reveals a CTG trinucleotide repeat expansion of 43 triplets in the JPH3 gene.
What is the cause of this gentleman’s symptoms?
CorrectIncorrect -
Question 8 of 28
8. Question
A three-year-old boy is brought to the neurology clinic following unexplained developmental delay and alterations in behaviour. He was born at term without complication. Early development was normal but slowed such that milestones were delayed from around 6 months old. He also developed sand-like crystal in his nappies. He was late sitting up and has great difficulty in crawling. He never progressed to walking. His speech is minimal.
Multiple involuntary muscle contractions are present include writhing motions, involuntary muscle contractions and arching of the spine. On examination, you note damage to the lips, tongue and fingertips. This has been investigated previously and thought to be self-injurious. There was evidence of spasticity, hyperreflexia and extensor plantars.
You are requesting a diagnostic genetic test.
A mutation in which gene fits best with these symptoms?
CorrectIncorrect -
Question 9 of 28
9. Question
A 35-year-old male is seen in the outpatient clinic with abnormal movements and difficulties feeding. He has a past medical history of anxiety, paranoia and learning difficulties and takes risperidone 2mg once daily.
During conversation, you note some vocal tics (grasping, sighing, whistling), repetitive tongue protrusions, orofacial dyskinesias, dysarthria and chorea. On formal examination you note bradykinesia, rigidity and subtle impairment in vertical upgaze. He was also overly friendly and, at times, socially inappropriate during the consultation. He scored 24/30 in the MoCA with impaired executive function and memory.
Blood tests show normal liver function with others pending and an MRI-brain, performed previously, revealed caudate head atrophy and dilatation of the anterior horns of the lateral ventricles.
What is likely diagnosis?
CorrectIncorrect -
Question 10 of 28
10. Question
A 34-year-old female presents to the emergency department with confusion, sweating and rigidity. She has a past medical history of schizophrenia and has recently started risperidone.
Her examination reveals a resting heart rate of 130 beats per minute, blood pressure 160/110mmHg, temperature 38.1°C and respiratory rate of 22/minute. Her GCS is 7 (M3 V2 E2), she is rigid in all four limbs and is markedly diaphoretic. The intensivist doctors have been called to assist.
There is no note of drug intoxication – although a toxicology screen has been sent – and her bloods show a white cell count of 14×109/L and creatine kinase 1100 U/L but there is no clear infective source and a pregnancy test is negative.
You commence IV fluids and stop her anti-psychotic due to concern about neuroleptic malignant syndrome (NMS).
What is the next line of management for NMS?
CorrectIncorrect -
Question 11 of 28
11. Question
A 24-year-old female presents with confusion and sweating. She has a past medical history of borderline personality disorder and there is speculation that she may have overdosed on an unknown drug around 6 hours ago according to her mother.
On examination, she is restless and markedly diaphoretic with a resting heart rate of 124 beats per minute, blood pressure 152/110mmHg, temperature 38.1°C and respiratory rate of 21/minute. Her GCS is 10 (M5 V3 E2) and her neurological exam reveals a tremor of the hands at rest and during action, hyperreflexia, ankle clonus, limb rigidity and extensor plantars. There are additional muscle jerks throughout the consultation but no clear epileptic features beyond this.
Her CT-brain is normal and bloods reveal a CK of 1000U/L and white cell count of 11 with no source of infection identified. Her pregnancy test is negative, ECG shows a sinus tachycardia and normal QTc interval and her blood paracetamol and salicylate levels are normal. A toxicology screen is normal.
What is the most likely cause?
CorrectIncorrect -
Question 12 of 28
12. Question
A 38-year-old man attends the neurology clinic accompanied by his parents with a 2-year history of resting tremor, bradykinesia and rigidity.
Examination is notable for dystonic posturing in both hands, symmetrical mild-moderate parkinsonism, ataxia and dysarthria. He attends in a wheelchair and has not walked independently for many years.
Past medical history includes intellectual disability and long-standing axonal neuropathy. There is no known family history. He takes no regular medication.
MR brain demonstrates cerebellar atrophy and brain iron accumulation in the globus pallidus, substantia nigra, and striatum.
Which of the following is the most likely diagnosis:
CorrectIncorrect -
Question 13 of 28
13. Question
Which of the following signs is not seen in neuroleptic malignant syndrome?
CorrectIncorrect -
Question 14 of 28
14. Question
Which of the following antiepileptics has not been associated with the development of chorea?
CorrectIncorrect -
Question 15 of 28
15. Question
Which of the following is most accurate in relation to the typical clinical manifestations of Huntington’s disease?
CorrectIncorrect -
Question 16 of 28
16. Question
A 32-year-old male is admitted to the Emergency Department with weakness and sensory disturbance following a severe gastrointestinal illness involving vomiting, abdominal pain and diarrhoea, a few weeks earlier. He is a smelter by trade. He has no past medical history but did have to take nitrofurantoin for a recent urinary infection, which is being followed up accordingly.
On examination, he has symmetrical weakness 4/5 with diminished reflexes throughout. You also notice an additional feature highlighted in the figure below.

What treatment should be started?
CorrectIncorrect -
Question 17 of 28
17. Question
Which of the following drugs is not associated with a significant anticholinergic effect?
CorrectIncorrect -
Question 18 of 28
18. Question
Which one of the following spinocerebellar ataxias (SCA) is associated with a pure cerebellar ataxia?
CorrectIncorrect -
Question 19 of 28
19. Question
Which of the following toxic compounds side effects are most likely to include abdominal pain, confusion, memory loss, and mood disorders?
CorrectIncorrect -
Question 20 of 28
20. Question
Which heavy metal chelator is commonly used for the treatment of mercury poisoning?
CorrectIncorrect -
Question 21 of 28
21. Question
Which of the following toxins is commonly associated with the neurological symptoms of seizures, ataxia, hallucinations, and encephalopathy?
CorrectIncorrect -
Question 22 of 28
22. Question
A 45-year-old male presents to the emergency department with hearing and balance issues. He reports his imbalance and vertigo can be induced by loud noises and his own speech is heard very loud in his right ear. He describes spinning vertigo and pulsatile tinnitus on the right.
Which of the following is the investigation most likely to secure the diagnosis?
CorrectIncorrect -
Question 23 of 28
23. Question
52-year-old female attends the Emergency Department with a 2-day history of “light-headedness”. On more specific questioning, she reports feeling like she is walking on a moving ship.
What examination finding would be most in keeping with a central cause for vertigo?
CorrectIncorrect -
Question 24 of 28
24. Question
A patient attends your clinic with a complaint of intermittent vertigo, exacerbated by movement. You suspect otoconia in the left horizontal semicircular canal.
You perform a modified Dix-Hallpike manoeuvre (supine roll test).
Which of the following would confirm your suspicions?
CorrectIncorrect -
Question 25 of 28
25. Question
You are referred a lady with a diagnosis of relapsing-remitting MS. Her main complaint is that of urinary frequency and urgency with nocturia. You perform a pre- and post-void ultrasound. The patient has the urge to urinate at a bladder volume of 120ml and there is no detectable urine remaining in the bladder after micturition.
An MRI of the spinal cord demonstrates no lesions, but an MRI of the brain shows multiple periventricular and juxtacortical lesions with further lesions in the cerebellar white matter and dorsal pons.
Which of the following treatments is the most appropriate at this stage?
CorrectIncorrect -
Question 26 of 28
26. Question
A 33-year-old male is referred to the Urology department for investigation of recurrent urinary tract infections and poor stream. A post-void bladder scan reveals a residual volume of 170ml.
A normal flow cystometry readout is shown (top image) and compared with the patient’s (below):
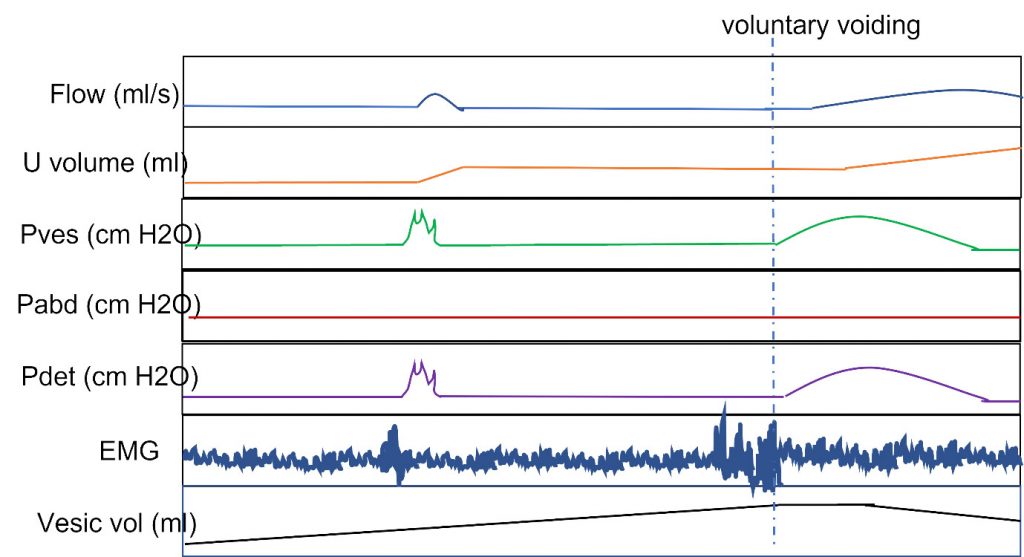
(U volume = volume of urine excreted; Pves = vesicular pressure; Pabd = abdominal pressure; Pdet = detrusor pressure; EMG = urethral sphincter EMG; Vesic vol = bladder volume)
A tumour at which of the following locations is likely to be responsible for his symptoms?
CorrectIncorrect -
Question 27 of 28
27. Question
You are asked to review a 25-year-old lady on the Obstetric ward. She had an elective Caesarean section 48 hours previously with a spinal anaesthetic and the procedure was uncomplicated.
Now she has regained full sensation in the lower limbs but has not been able to pass urine since removal of her catheter over 24 hours ago. A bladder scan revealed over 1L of urine in the bladder and an in-out catheter passed 6 hours ago relieved a volume of 1.2L.
She does not describe any pain, other than some soreness around the Caesarean incision site. She does not report any urge to pass urine
Medical history is remarkable only for infrequent migraine. She is taking 30mg dihydrocodeine TDS since the surgery but is otherwise on no regular medications.
On examination she has a palpable bladder. Upper limb examination is unremarkable. Power in the lower limbs is 5/5 on the MRC scale, although hip flexion is limited by pain. Reflexes are intact. There is subjective reduction in pin-prick sensation distally but no sensory level and a 512Hz tuning fork is detected at the metatarsophalangeal joint.
Which of the following investigations is most likely to confirm the underlying diagnosis?
CorrectIncorrect -
Question 28 of 28
28. Question
A 3-month-old boy is noted by his parents to be floppy and have ‘abnormal eye movements’. His parents specifically report poor head control and he is yet to smile.
On examination, there is multi-directional nystagmus in multiple eccentric gazes, hypotonia, global ataxia and head tremor.
An MRI brain is performed and shown below.
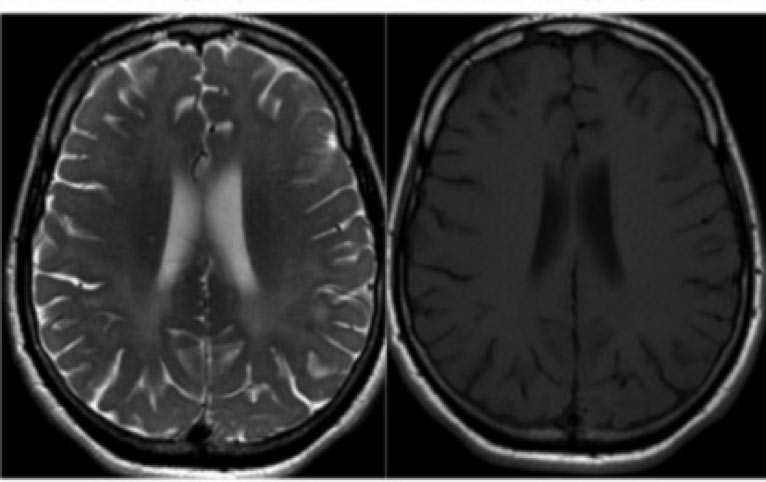
A genetic leukodytrophy panel is subsequently sent which reveals a mutation in the PLP1 gene.
What is the diagnosis?
CorrectIncorrect

The wording on 15 is a little clumsy – while you could argue inverse correlation is a form of correlation, leaving the potential for this misunderstanding seems unnecessary